This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 23 year old female patient store manager by occupation came to general medicine OPD with
CHIEF COMPLAINTS
• Pain in the left side of abdomen on and off since 1 year
HISTORY OF PRESENTING ILLNESS
• Patient was apparently asymptomatic a year back then she started developing pain in left hypochondrium which is insidious in onset intermittent & dragging type. since last one year she is having 1-2episodes of pain every month lasting for 30-60 min.
•c/o frequent onset of fever (once in 15-20 days) since 1 year, for which she visited a local hospital and found to be having low hemoglobin & started oral iron (used for one month) for which she had black coloured stools.
•c/o shortness of breath since one year ( Grade III)
•c/o early fatigability,
•decreased appetite since 14 years of age
•No H/o chest pain, pedal edema
•No H/o orthopnea, PND
•No H/o cold , cough
•No bleeding manifestations
•No c/o weight loss
PAST HISTORY
•Not a known case of Hypertension , Diabetes mellitus , Tuberculosis , asthma , thyroid disorders, epilepsy , CVD , CAD
• No H/o surgeries in the past
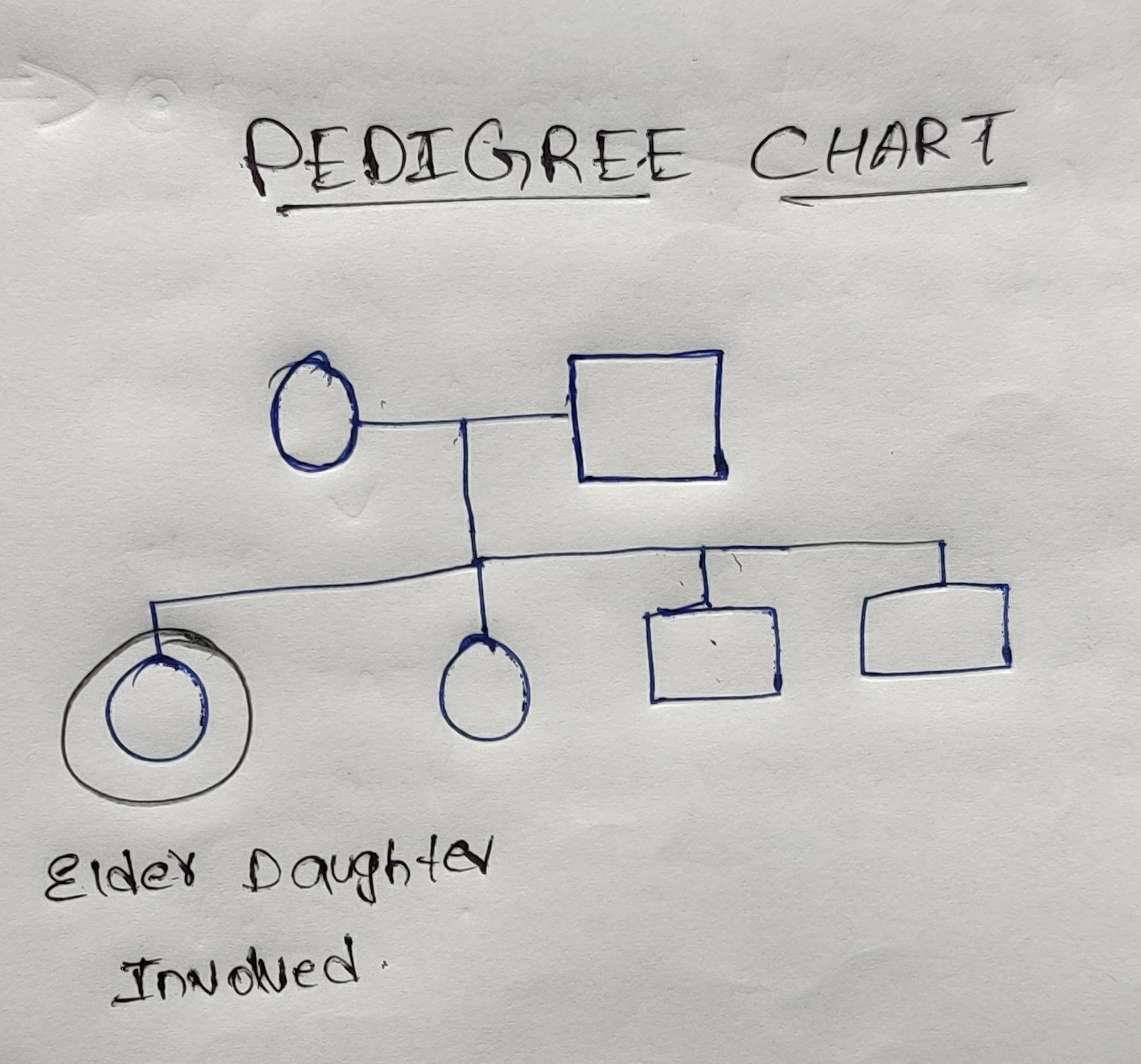
FAMILY HISTORY
•No significant family history
PERSONAL HISTORY
• Diet - mixed
• appetite - decreased
• sleep - adequate
• bowel and bladder - regular
• No addictions and no known allergies
MENSTRUAL HISTORY
• age of menarche - 12 yrs
• Regular cycles , 3/28 , changes 3-4 pads per day.
• No gynecological problems
GENERAL PHYSICAL EXAMINATION
• patient is conscious, coherent, cooperative and well oriented to time, place and person.
• moderately nourished
• No pallor, icterus, cyanosis, clubbing, lymphadenopathy,edema.
VITALS
Temperature : afebrile
Respiratory Rate:18 cycles per minute
Pulse rate : 78 bpm
Blood pressure :110/70 mmHg
SYSTEMIC EXAMINATION
PER ABDOMEN :
• inspection
Shape - flat , no distention
Umblicus - inverted, round scar around umblicus
No visible pulsations,peristalsis, dilated veins
Visible swelling in the left hypochondrium , 6cm×4cm in size, oval shape, smooth, skin over swelling is normal
Hernial orifices are free
• Palpation
No local rise of temperature and tenderness
Spleen palpable ( moderate splenomegaly) 5cm below it's costal margin by
CLASSICAL METHOD
Other methods
Dipping method(in ascites)
Bimanual method
No palpable liver
•Percussion
liver span -12 cm
Spleen - dullness extending to umbilical region
Fluid thrill and shifting dullness absent
Auscultation
Bowel sounds: present
CARDIOVASCULAR SYSTEM:
•Inspection
Shape of chest- elliptical shaped chest
No engorged veins, scars, visible pulsations
•Palpation
Apex beat can be palpable in 5th inter costal space medial to mid clavicular line
No thrills and parasternal heaves can be felt
•Auscultation
S1,S2 are heard
no murmurs
RESPIRATORY SYSTEM:
•Inspection
Shape of the chest : elliptical
B/L symmetrical ,
Both sides moving equally with respiration
No scars, sinuses, engorged veins, pulsations
•Palpation
Trachea - central
Expansion of chest is symmetrical.
•Auscultation
B/L air entry present . Normal vesicular breath sounds
CNS:
•HIGHER MENTAL FUNCTIONS-
Normal
Memory intact
•CRANIAL NERVES :Normal
•SENSORY EXAMINATION
Normal sensations felt in all dermatomes
•MOTOR EXAMINATION
Normal tone in upper and lower limb
Normal power in upper and lower limb
Normal gait
•REFLEXES
Normal, brisk reflexes elicited- biceps, triceps, knee and ankle reflexes elicited
•CEREBELLAR FUNCTION
Normal function
No meningeal signs were elicited
•Provisional diagnosis:-
Splenomegaly with anemia.
4/03/2023
HAEMOGLOBIN- 8.7 gm/dl
TOTAL COUNT - 2130 cells/cumm
pcv - 30.0
MCV - 78.9
MCHC - 28.6
smear- Anisocytosis with normocytes microcytes tear drops pencil forms and macrocytes
impressions -Pancytopenia
7/03/2023
HAEMOGLOBIN- 9.2 gm/dl
TOTAL COUNT - 2000 cells/cumm
pcv - 33.4
MCV - 82.1
MCHC - 27.5
smear- Anisocytosis with normocytes microcytes tear drops pencil forms and macrocytes
impressions -Pancytopenia
9/03/2023
HAEMOGLOBIN- 9.8 gm/dl
TOTAL COUNT - 2600 cells/cumm
pcv - 34.3
MCV - 80
MCHC - 28.6
smear- Anisocytosis with normocytes microcytes tear drops pencil forms and macrocytes
impressions -Pancytopenia
12/03/2023
HAEMOGLOBIN- 8.8 gm/dl
TOTAL COUNT - 2000 cells/cumulative
lymphocytes - 42%
pcv - 30.1
MCV - 80.3
MCH - 23.5
MCHC - 29.5
RBC 3.75 millions/cumm
smear- Anisocytosis with normocytes, microcytes tear drops ,pencil forms and macrocytes
impressions -Pancytopenia
13/03/2023
HAEMOGLOBIN- 8.7 gm/dl
TOTAL COUNT - 2000 cells/cumm
pcv - 29.8
MCV - 80.5
MCH - 23.5
MCHC - 29.5
RBC - 2.70millions /cumm
smear- Ansocytosis with normocytes microcytes tear drops pencil forms and macrocytes
impressions -Pancytopenia
APTT
Result- 41s
BLOOD UREA- 26 mg/dl
BLEEDING AND CLOTING TIME
bleeding time - 2min
clotting time -4min
BLOOD GROUPING AND RH TYPE-B positive
PROTHROMBIN TIME- 2.0sec
SERUM CREATININE - 0.6 mg/dl
HIV - non reactive
Anti HCV antibodies -non reactive
USG
Bone marrow biopsy
Final Diagnosis : splenomegaly with pancytopenia
TREATMENT :-
•tab LIVOGEN - 150mg OD
•tab ULTRACET -500mg TID







Comments
Post a Comment